A peptic ulcer is an open sore or raw area in the lining of the stomach or intestine.
- A gastric ulcer occurs in the stomach.
- A duodenal ulcer occurs in the first part of the small intestine.

Normally, the lining of the stomach and small intestines can protect itself against strong stomach acids. But if the lining breaks down, the result may be:
- Swollen and inflamed tissue, called (gastritis)
- An ulcer
 Watch this video about:Stomach ulcer
Watch this video about:Stomach ulcer
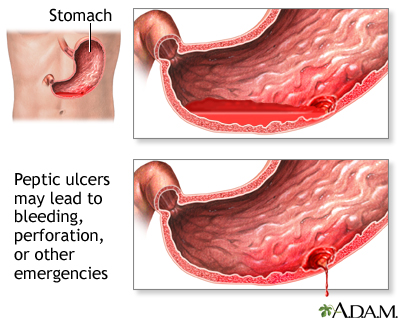
Most ulcers occur in the first layer of the inner lining. A hole that goes all the way through the stomach or duodenum is called a perforation. A perforation is a medical emergency.
The most common cause of ulcers is infection of the stomach by bacteria called Helicobacter pylori(H.pylori). Most people with peptic ulcers have these bacteria living in their digestive tract. Yet, many people who have these bacteria in their stomach do not develop an ulcer.
The following factors raise your risk for peptic ulcers:
- Drinking too much alcohol
- Regular use of aspirin, ibuprofen, naproxen, or other nonsteroidal anti-inflammatory drugs (NSAIDs). Taking aspirin or NSAIDs once in a while is safe for most people.
- Smoking cigarettes or chewing tobacco
- Being very ill, such as being on a breathing machine
- Having radiation treatments
A rare condition called Zollinger-Ellison syndrome causes stomach and duodenal ulcers.

Many people believe that stress causes ulcers. It is not clear if this is true for normal stress.
Small ulcers may not cause any symptoms. Some ulcers can cause serious bleeding.
Abdominal pain is a common symptom. The pain can differ from person to person, and some people have no pain.
Other symptoms include:
- Feeling of fullness and problems drinking as much fluid as usual
- Hunger and an empty feeling in the stomach, often 1 to 3 hours after a meal
- Mild nausea that may go away with vomiting
- Pain or discomfort in the upper abdomen
- Pain in the upper abdomen that wakes you up at night
Other possible symptoms include:
- Bloody or dark tarry stools
- Chest pain
- Fatigue
- Vomiting, possibly bloody
- Weight loss
To diagnose an ulcer, you may need a test called an upper endoscopy (EGD).
- This is a test to examine the lining of the esophagus (the tube that connects your throat to your stomach), stomach, and first part of the small intestine.
- It is done with a small camera (flexible endoscope) that is inserted down the throat.
- This test most often requires sedation given through an IV

Upper endoscopy is done on most people when peptic ulcers are suspected or when you:
- Have a low blood count (anemia)
- Have trouble swallowing
- Are vomiting blood or your stools are blood or dark and tarry looking
- Have been losing weight without trying
Testing for H. pylori is also needed.
Other tests you may have include:
- Hemoglobin blood test to check for anemia
- Stool occult blood test to test for blood in your stool
Sometimes, you may need a test called an upper GI series. A series of x-rays are taken after you drink a thick substance called barium. This does not require sedation.
In order for your ulcer to heal and to reduce the chance it will come back, you will be given medicines to:
- Kill the H. pylori bacteria (if present)
- Reduce acid levels in the stomach
Take all of your medicines as you have been told. Other changes in your lifestyle can also help.
If you have a peptic ulcer with an H. pylori infection, the standard treatment uses different combinations of the following medicines for 7 to 14 days:
- Two different antibiotics to kill H. pylori
- Proton pump inhibitors such as omeprazole (Prilosec), lansoprazole (Prevacid), or esomeprazole (Nexium)
- Bismuth (the main ingredient in Pepto-Bismol) may be added to help kill the bacteria
If you have an ulcer without an H. pylori infection, or one that is caused by taking aspirin or NSAIDs, you will likely need to take a proton pump inhibitor for 8 weeks.
You may also be prescribed this type of medicine regularly if you must continue taking aspirin or NSAIDs for other health conditions.
Other medicines used for ulcers are:
- Misoprostol, a drug that may help prevent ulcers in people who take NSAIDs on a regular basis
- Medicines that protect the tissue lining (such as sucralfate)
If a peptic ulcer bleeds a lot, an EGD may be needed to stop the bleeding. Methods used to stop the bleeding include:
- Injecting medicine in the ulcer
- Applying metal clips to the ulcer
Surgery may be needed if:
- Bleeding cannot be stopped with an EGD
- The ulcer has caused a tear
Peptic ulcers tend to come back if untreated. There is a good chance that the H. pylori infection will be cured if you take your medicines and follow your health care provider's treatment advice. You will be much less likely to get another ulcer.
Complications may include:
- Severe blood loss
- Scarring from an ulcer may make it harder for the stomach to empty
- Perforation or hole of the stomach and intestines
Get medical help right away if you:
- Develop sudden, sharp abdominal pain
- Have a rigid, hard abdomen that is tender to touch
- Have symptoms of shock, such as fainting, excessive sweating, or confusion
- Vomit blood or have blood in your stool (especially if it is maroon or dark, tarry black)
Call your health care provider if:
- You feel dizzy or light-headed
- You have ulcer symptoms
Avoid aspirin, ibuprofen, naproxen, and other NSAIDs. Try acetaminophen instead. If you must take such medicines, talk to your provider first. Your provider may:
- Test you for H. pylori before you take these medicines
- Have you take proton pump inhibitors (PPIs) or an acid blocker
- Have you take a drug called misoprostol
The following lifestyle changes may help prevent peptic ulcers:
- DO NOT smoke or chew tobacco.
- Limit alcohol to no more than two drinks per day.
Ulcer - peptic; Ulcer - duodenal; Ulcer - gastric; Duodenal ulcer; Gastric ulcer; Dyspepsia - ulcers
Chan FKL, Lau JYW. Peptic ulcer disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran's Gastrointestinal and Liver Disease. 9th ed. Philadelphia, PA: Elsevier Saunders; 2010:chap 53.
Chey WD, Wong BC. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102:1808-25. PMID: 17608775www.ncbi.nlm.nih.gov/pubmed/17608775.
Kuipers EJ, Blaser MJ. Acid peptic disease. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier Saunders; 2011:chap 141.
Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012 Mar;107(3):345-60. PMID: 22310222 www.ncbi.nlm.nih.gov/pubmed/22310222.
Lanza FL, Chan FK, Quigley EM; Practice Parameters Committee of the American College of Gastroenterology. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009 Mar;104(3):728-38.
McColl KEL. Helicobacter pylori infection. NEJM. 2010;362:1597-1604. PMID: 20427808www.ncbi.nlm.nih.gov/pubmed/20427808.






Nice post. Well what can I say is that these is an interesting and very informative topic on gastric lining inflammation
ReplyDelete