Duodenal Stenosis and Atresia
Embryology
The hepatobiliary system and pancreas form during the third week of gestation, as the second portion of the duodenum gives rise to biliary and pancreatic buds at the junction of the foregut to the midgut. The duodenum also undergoes a solid phase during this time; between 8-10 weeks' gestation, the duodenal lumen is reestablished by the gathering of vacuoles, and recanalization occurs.
Insults during this crucial period of development are believed to result in failure of recanalization and consequent atresias, stenoses, and webs. In addition, duodenal atresias have been associated with a closely surrounding piece of pancreatic tissue. Whether this tissue is an annular pancreas or merely a failure of duodenal development is debatable.[1, 2]
Classification
A stenosis is an incomplete obstruction with a small opening secondary to a diaphragm or web, whereas an atresia is a complete obstruction. Unlike other intestinal atresias, duodenal atresias are associated with other congenital anomalies. Approximately 50% of patients with duodenal atresias have some form of anomaly (eg, cardiac, anorectal, or genitourinary), and as many as 40% have trisomy 21.[3, 4, 5]
Esophageal atresia and the VATER (ie, vertebral defects, anal atresia, tracheoesophageal fistula with esophageal atresia, and renal and radial anomalies) syndrome have also been associated with duodenal atresia.[6] Hence, all neonates with duodenal atresia should be assessed for concomitant malformations. Growth retardation and polyhydramnios are often present prenatally.
Anatomically, most congenital duodenal obstructions are considered periampullary, with the biliary outlet occurring proximal or distal to the site of obstruction. The degree of obstruction dictates the amount of resulting pathology. The obstruction causes dilation of the proximal duodenum and stomach, as well as hypertrophy and distention of the pylorus.
A common variation is the windsock anomaly, in which the duodenum is dilated distal to the point of obstruction because of a prolapsing membrane or web (see the image below). This may be confused with a more distal duodenal obstruction.
Diagnosis
Prenatal ultrasonography may indicate structural and associated abnormalities, such as a dilated stomach and proximal duodenum. Polyhydramnios is suggestive of a proximal gastrointestinal (GI) tract obstruction because the fetus is unable to swallow the amniotic fluid. Common associated anomalies and chromosomal defects may be assessed by screening maternal serum and amniotic fluid.
In the newborn, clear or bilious emesis is evident within hours of birth, with or without abdominal distention. An output of more than 20 mL of gastric contents is indicative of possible obstruction.[7] Because of incomplete obstruction, patients with a stenosis or web may present later with dehydration or failure to thrive.
Plain radiography (see the first image below) is helpful and may reveal the classic double-bubble sign, representing air in the stomach and proximal duodenum, which is associated with complete or near-complete duodenal obstruction. Upright and contrast radiography using air or contrast may confirm the diagnosis (see the second image below). Malrotation with volvulus may also result in duodenal obstruction with a double-bubble sign and can coexist with duodenal atresia in as many as 30% of cases.[8]
Treatment
Gastric decompression is essential to prevent aspiration, and thermoregulation should be monitored at all times. Unless malrotation with volvulus remains a concern, preoperative assessment of other associated anomalies should be performed. When fluid resuscitation and a full assessment have been accomplished, the neonate may proceed to surgery.
The following two basic options are available for repair of duodenal obstruction secondary to a web or atresia:
- Duodenoduodenostomy
- Duodenotomy with excision of the web
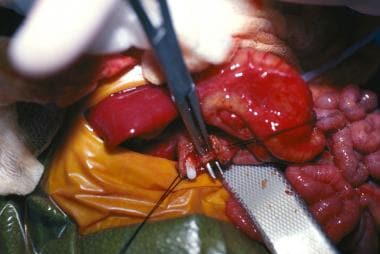
The most common repair is a duodenoduodenostomy. The classic approach is through a supraumbilical transverse abdominal incision that provides adequate exposure of the duodenum once the ascending and transverse colon are mobilized to the left. A catheter is inserted through the stomach to help define the site of obstruction.
In addition, the entire small bowel is carefully explored for other sites of obstruction. Care is taken to examine the gallbladder to ensure that a preduodenal portal vein is not evident and to locate the ampulla of Vater to avoid inadvertent injury. Laparoscopy has also been shown to be a safe and effective approach to repair of congenital duodenal obstruction.[9, 10, 11, 12]
The proximal duodenum is usually dilated as compared with the thin-walled, flat distal duodenum and jejunum. A diamond-shaped anastomosis may be fashioned between a longitudinal incision in the distal collapsed end of the duodenum and a transverse incision in the inferior aspect of the bulbous blind-ended proximal duodenum. In the laparoscopic approach, U-clips are used for the duodenoduodenostomy.[9] The proximal duodenum is sometimes tapered by plicating its lateral antimesenteric side. A Ladd procedure is warranted if malrotation is present.
If a web is present, duodenotomy with excision of the web may be performed instead of duodenoduodenostomy. The web should be defined with the aid of a tube through the stomach, and the ampulla of Vater should be carefully identified before excision. A longitudinal incision is then made directly on the web, and the web is excised. The duodenum is then closed transversely, to avoid narrowing.
Feeding may be started when GI function is established. In some patients, this may take as long as 2 weeks. Gastric decompression via a nasogastric tube is required until that time.
Outcome
Anastomotic leakage, injury to the bile duct, and sepsis are early complications. Late complications include peptic ulceration secondary to alkaline reflux, blind-loop syndrome due to duodenal stasis, and recurrent obstruction.[13, 14, 15] In one series, as many as 12% of patients had late complications requiring reoperation for a number of reasons, including reflux and peptic ulcer disease, associated biliary abnormalities, and bowel obstruction.[8]
The prognosis is good after repair of duodenal stenosis or atresia; however, coexisting diagnoses (eg, Down syndrome and cardiac anomalies) affect outcome.[16, 17] Long-term data showed that a 9% combined early and late mortality over an average 6-year follow-up period was due almost exclusively to associated congenital anomalies.[8] In addition, birth weight is a predictor of mortality. Infants with duodenal atresia who weigh less than 2 kg at birth have poorer survival, regardless of the presence of other congenital abnormalities.[18]








0 التعليقات:
Post a Comment